Keep urine warm with simple, effective methods by using insulated containers, heat activators, or body heat, ensuring it remains at a stable temperature for various needs like medical testing or personal comfort. These techniques are practical and easy to implement.
It’s a common concern, especially when you need to collect a sample for medical reasons. The thought of urine cooling down before it reaches its destination can be worrying. This guide is here to banish that stress! We’ll walk you through easy, proven ways to keep your urine at the right temperature, making the process smooth and successful.
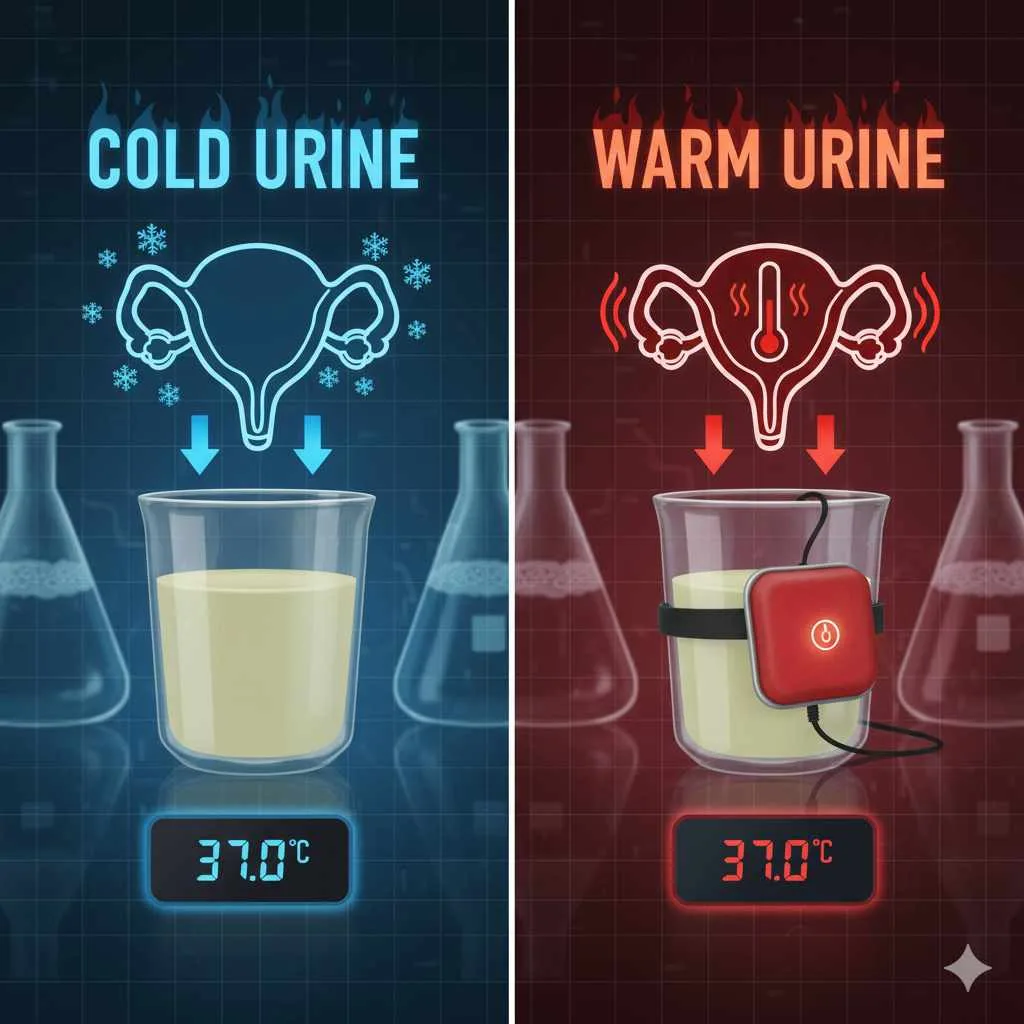
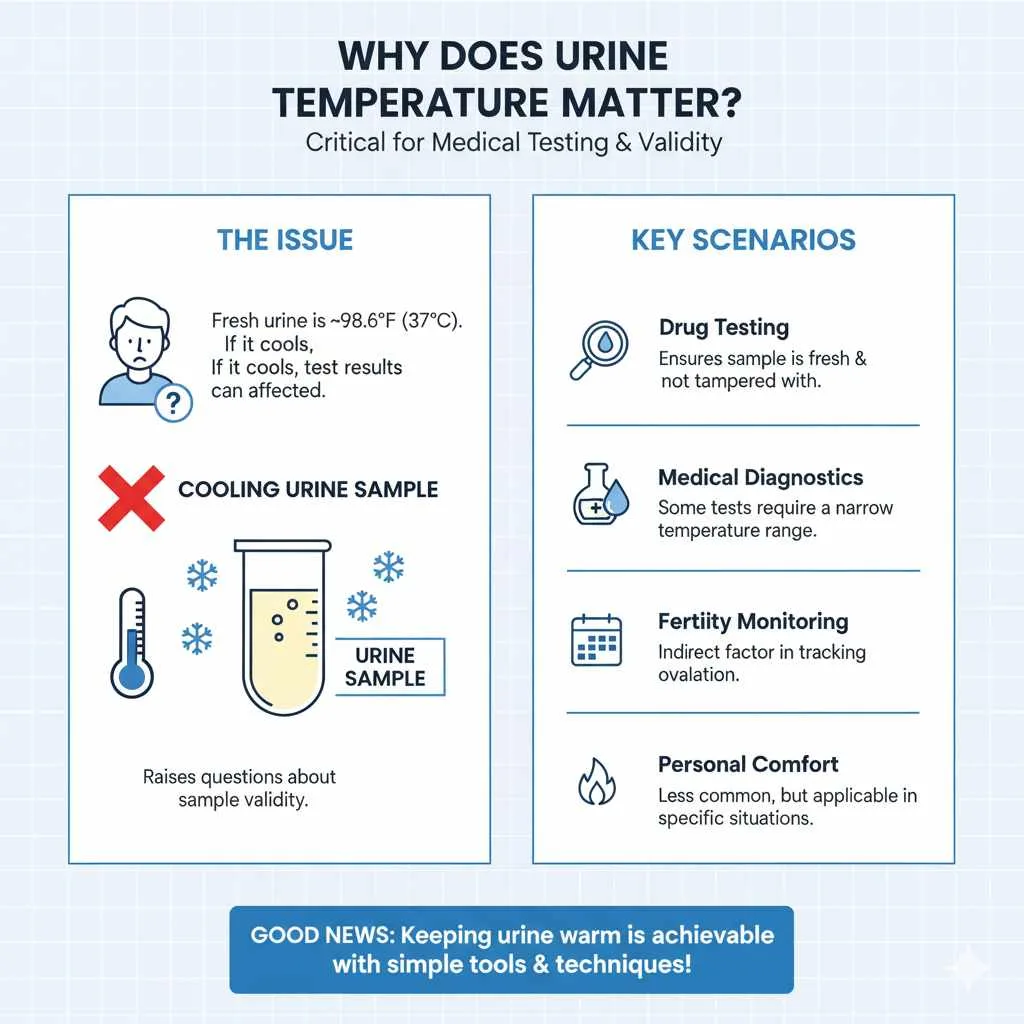
Why Does Urine Temperature Matter?
You might be wondering, “Why all the fuss about warm urine?” For many situations, especially medical testing, the temperature of a urine sample is a critical factor. Fresh urine is typically around body temperature, which is about 98.6°F (37°C). If it cools too much, it can affect test results, leading to unnecessary complications or retesting.
Think of it like delivering a delicate item – it needs to arrive in the best possible condition. For certain medical tests, like drug screening or specific diagnostic analyses, temperature is a key indicator of recent sample collection. A sample that’s too cold might raise questions about its validity.
Common Scenarios Where Urine Temperature is Important:
- Drug Testing: A primary reason for checking urine temperature is to ensure the sample is fresh and hasn’t been tampered with or substituted.
- Medical Diagnostics: Some tests need to be performed on a sample within a narrow temperature range to ensure accuracy.
- Fertility Monitoring: In some fertility treatments or natural family planning methods, tracking ovulation involves checking body temperature, and sample temperature can be an indirect factor.
- Personal Comfort: While less common, some individuals might seek methods for personal warmth in specific situations.
The good news is that keeping urine at the correct temperature isn’t complicated. With a few simple tools and techniques, you can ensure your sample is ready when you need it.
Understanding Ideal Urine Temperature Ranges
For most laboratory tests, the acceptable temperature range for a urine sample is quite specific, usually mirroring body temperature. Laboratories often have strict guidelines to ensure accuracy and prevent fraud, especially in situations like workplace drug testing. According to the U.S. Department of Health and Human Services (HHS), a urine specimen must be tested for temperature within 4 minutes of collection, and the acceptable range for verification is between 90°F (32.2°C) and 100°F (37.8°C).
Exceeding these limits can lead to a test being flagged as invalid. This is why understanding how to maintain that ideal temperature is so crucial. It’s not just about warmth; it’s about accuracy and reliability. Even a few degrees can make a difference in a scientific context.
Factors Affecting Urine Temperature
- Ambient Temperature: The temperature of the room or environment where the sample is collected and stored will cause it to cool down. A cold room will cool it faster.
- Time Delay: The longer the time between collection and testing, the more the urine will cool.
- Container Material: Some container materials might insulate better than others, but most standard collection cups offer minimal thermal protection.
Knowing these factors helps us strategize the best methods to counteract them.
Proven Methods to Keep Urine Warm
Here are several reliable techniques, ranging from simple to slightly more involved, that you can use to keep your urine at the desired temperature. We’ll cover what you need and how to use each method effectively.
Method 1: The Power of Insulation
Insulation is your best friend when trying to maintain temperature. By creating a barrier around the collection container, you slow down the rate at which the urine loses heat.
What You’ll Need:
- A clean urine collection cup (often provided by the testing facility)
- An insulating material:
- A small thermos or insulated travel mug
- A neoprene sleeve (like those for water bottles)
- A clean, thick sock or a few layers of paper towels
- A small cooler bag
How to Do It:
- Prepare Your Container: If you’re using a standard collection cup, ensure it’s clean. If you’re using a thermos or insulated mug, make sure it’s also clean and dry.
- Collect the Sample: Collect the urine directly into your chosen container. For optimal temperature, collect the “mid-stream” portion of the urine flow, as this is closest to body temperature.
- Insulate Immediately: As soon as you’ve collected enough, seal the container. If using a cup, immediately place it into your insulating material.
- Thermos/Insulated Mug: Place the sealed urine collection cup directly inside the thermos or mug. This creates a double layer of insulation.
- Neoprene Sleeve/Sock/Paper Towels: Wrap the sealed collection cup snugly with the neoprene sleeve, sock, or several layers of paper towels. Secure with a rubber band or tape if needed.
- Cooler Bag: If you have a small cooler bag, place the sealed collection cup inside this.
- Maintain Proximity: Keep the insulated container close to your body if possible. Your body provides a consistent source of warmth that the insulation will help trap.
Pro Tip: For medical tests, always follow the specific instructions provided by the clinic or laboratory. They may have restrictions on what you can bring or how you can transport the sample.
Method 2: Using a Warming Device
For situations requiring a more precise or sustained warmth, specialized warming devices can be very effective. These are designed to provide a consistent temperature source.
Types of Warming Devices:
- Chemical Hand Warmers (Single-Use): These are small, air-activated packs that generate heat for several hours.
- Electric Warming Pads (Portable): Some battery-operated pads can maintain a specific temperature, though these are less common for personal use with urine samples due to practicality.
- Therapeutic Heat Packs: Reusable heat packs that can be warmed in a microwave or by hot water.
How to Use Chemical Hand Warmers:
- Activate the Warmer: Open the hand warmer package and shake it or expose it to air according to its instructions. It will begin to heat up.
- Attach (Carefully!): Once the hand warmer has reached a warm, not hot, temperature (test on your hand first!), you can place it outside the collection container, secured to its side. Do NOT place it inside the container with the urine.
- Insulate Further: Wrap the container with the hand warmer attached using additional insulating material like a sock, paper towels, or a neoprene sleeve. This helps distribute the heat evenly and prevents it from getting too hot.
- Monitor Temperature: For critical tests, it’s essential to check the temperature periodically if possible, or ensure the hand warmer will last until transport.
Important Note: Be extremely careful not to overheat the sample. Urine that is too hot (above HHS guidelines) is as invalid as urine that is too cold. The goal is to maintain it within the acceptable range, ideally close to body temperature.
Method 3: Body Heat Transfer
Your own body is a reliable source of warmth. Using your body heat strategically can help maintain the temperature of your urine sample.
How to Do It:
- Secure the Container: Collect the sample in a clean cup.
- Seal and Insulate Lightly: Seal the cup. You can wrap it in a thin layer of paper towels or a cloth – just enough to provide a little buffer but still allow heat transfer.
- Carry Close to the Body: Place the wrapped collection cup in an inside pocket of your clothing (e.g., a jacket pocket or shirt pocket).
- Maintain Contact: Keep it in contact with your skin. The warmth from your body will transfer through the container and help keep the urine warm.
- Choose the Right Pocket: An inside pocket is ideal as it offers more protection from ambient air and is closer to your core body temperature.
Considerations: This method is best for shorter time frames and when you can keep the container consistently against your body. It’s less effective in very cold environments or if you need to transport the sample for an extended period without further warming.
Choosing the Right Method for Your Needs
The best method for you depends on several factors: how long you need to keep the urine warm, the ambient temperature, and the specific requirements of the test or situation.
Comparison Table: Warming Methods
| Method | Pros | Cons | Best For |
|---|---|---|---|
| Insulation (Thermos, Sleeve, Towels) | Simple, readily available materials, effective at slowing heat loss. | Doesn’t actively add heat, only preserves existing warmth. | Short to medium transport times, moderate temperatures. |
| Chemical Hand Warmers + Insulation | Provides active, sustained warmth. Relatively inexpensive. | Risk of overheating if not used carefully. Requires careful application. | Longer transport times, colder environments, requires precise temperature maintenance. |
| Body Heat Transfer | Free, always available, discreet. | Least effective in very cold or for long durations. | Short transport, mild temperatures, immediate post-collection. |
Factors to Consider When Selecting a Method:
- Timeframe: How long will it be between collection and when the temperature needs to be verified?
- Ambient Temperature: Will you be in a warm room or a cold car?
- Mobility: Will you be stationary, or moving around?
- Test Requirements: Are there specific instructions from the testing facility? Always prioritize these.
- Discretion: Some methods are more discreet than others.
Understanding specific temperature requirements for drug testing is essential, as many standardized procedures rely on this measurement to ensure sample integrity.
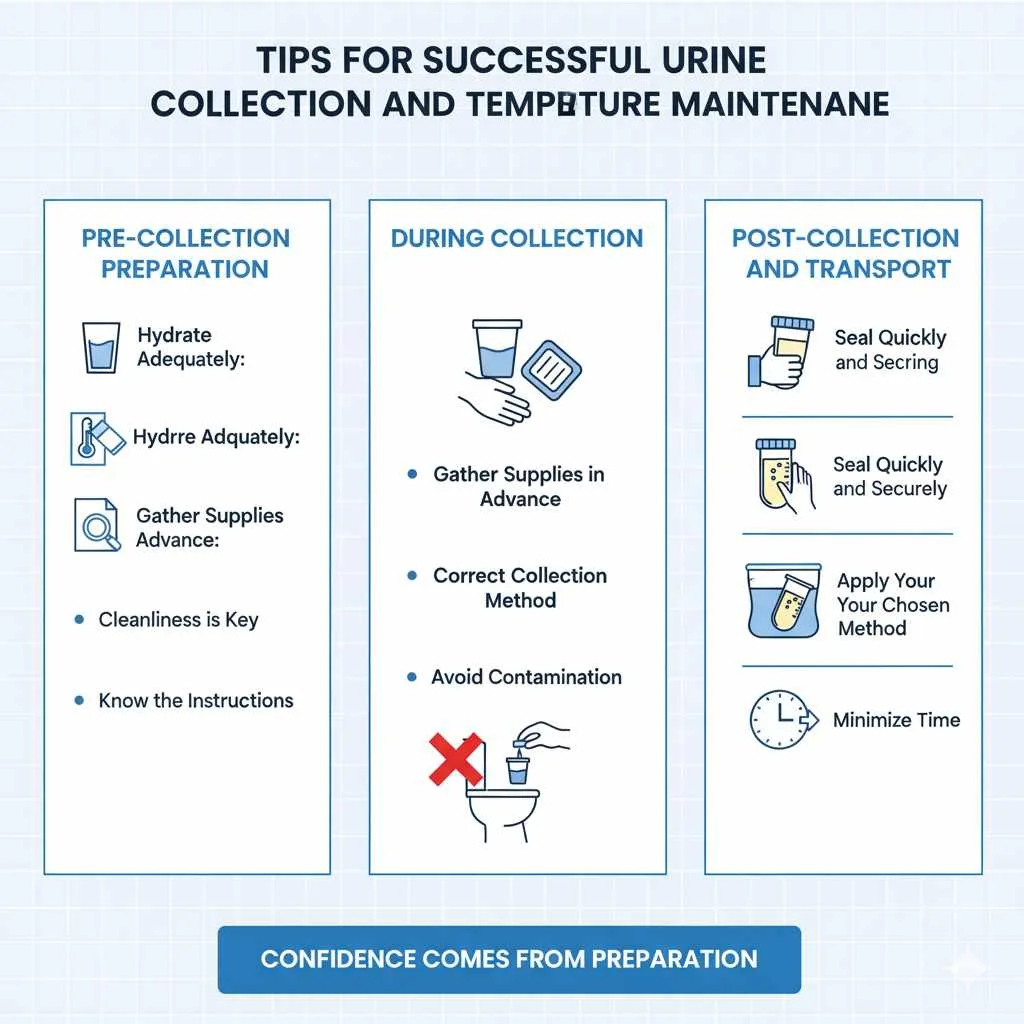
Tips for Successful Urine Collection and Temperature Maintenance
Beyond the chosen method, a few extra tips can make your urine collection and temperature maintenance process smoother.
Pre-Collection Preparation:
- Hydrate Adequately: Drink enough water a couple of hours before you anticipate needing to collect a sample. This ensures you can produce enough urine without it being too concentrated.
- Gather Supplies in Advance: Have your collection cup, chosen warming/insulating materials, and any necessary bags or containers ready before you need them.
- Know the Instructions: If this is for a medical test, thoroughly read and understand all instructions provided by the healthcare professional or lab.
During Collection:
- Cleanliness is Key: Ensure your hands are clean before handling the collection cup. Follow any instructions regarding cleaning the genital area before collection if provided.
- Correct Collection Method: For most tests, the “mid-stream” sample is preferred. This means starting urination into the toilet, then collecting the urine in the cup, and finishing urination into the toilet. This avoids initial and final urine which can contain more contaminants.
- Avoid Contamination: Try not to touch the inside of the collection cup or the lid. Do not let toilet water or other contaminants get into the sample.
Post-Collection and Transport:
- Seal Quickly and Securely: Once collected, immediately put the lid on the container and ensure it’s sealed tightly.
- Apply Your Chosen Method: Implement your insulation, warming gadget, or body heat technique right away.
- Minimize Time: Transport the sample to the testing facility as quickly as possible. The less time that passes, the easier it is to maintain temperature.
- Inform the Staff: If you’ve used a specific method to maintain temperature, it can be helpful to inform the lab technician upon arrival.
Remember, confidence comes from preparation. By planning and following these steps, you can manage this task effectively.
Frequently Asked Questions (FAQ)
Q1: How quickly does urine cool down?
Urine typically starts to cool immediately after leaving the body. In average room temperature (around 70°F or 21°C), it can drop several degrees Fahrenheit within just a few minutes. In colder environments, the cooling process is much faster.
Q2: Can I use a regular water bottle to keep it warm?
A standard plastic water bottle offers very little insulation. While it can provide a slight barrier, it’s not effective for maintaining urine temperature for any significant amount of time. Insulated containers like thermoses or specialized sleeves are much better choices.
Q3: What if the urine sample gets too hot?
If a urine sample tests outside the acceptable temperature range (typically 90°F to 100°F or 32.2°C to 37.8°C for drug tests), it can be considered invalid. This could lead to the test being rejected and requiring a re-collection, which can be inconvenient. It’s crucial to avoid overheating by using warming methods judiciously and testing temperature if unsure.
Q4: Is it okay to bring a pre-warmed bottle of water to dilute my sample if needed?
For most official drug testing, bringing anything to dilute your sample is strictly prohibited and considered tampering. Always follow the specific instructions given by the testing facility. If you are concerned about hydration for a test, discuss it with the administrator beforehand.
Q5: How can I keep a urine sample warm in very cold weather?
In very cold weather, a combination of methods is best. Start by collecting the urine and immediately using a chemical hand warmer secured outside the container, then wrap the entire package in multiple layers of towels or a thick sock, and finally, place it inside a small insulated bag or a thermos. Keeping it close to your body in an inside pocket can add an extra layer of warmth.
Q6: Do I need a special container to keep urine warm?
You don’t necessarily need a special container. Standard laboratory-provided collection cups can be used, but you must implement external warming and insulation methods to maintain their temperature. If a specialized container is required, it will usually be specified by the testing facility. For example, some breathalyzer kits or specialized lab tests might come with integrated temperature monitoring.
Conclusion
Navigating the nuances of urine temperature can seem daunting, but as we’ve explored, it’s a manageable aspect of sample collection. By understanding why temperature matters and employing simple, proven strategies—whether it’s the insulating power of everyday items, the targeted warmth of portable devices, or the discreet heat of your own body—you can confidently ensure your sample remains within the correct range.
Remember, preparation and following instructions are key. Having your supplies ready, collecting the sample correctly, and implementing your chosen warming method immediately can make all the difference. These techniques are not just for medical necessity; they offer practical solutions for maintaining a specific temperature when needed. With this knowledge, you’re well-equipped to handle urine collection and temperature maintenance with ease and success. Your comfort and the accuracy of the process are our top priorities!