Bakers Cyst vs Popliteal Cyst: The essential difference is really just the name! Both terms refer to the exact same fluid-filled lump that forms behind the knee. Understanding causes, symptoms, and simple home care is the key to managing this common, often uncomfortable swelling.
Have you ever noticed a strange bulge or tightness right behind your knee? Maybe it feels like a balloon filled with water, and walking or bending your leg makes it worse. This is a very common issue, and it often causes worry if you don’t know what it is. Many folks get confused when doctors use two different names: Baker’s Cyst or Popliteal Cyst. Don’t fret! We are going to clear this up simply. Think of me as your friendly mechanic guiding you through a strange noise under the hood—it’s usually an easy fix once you know the parts. We’ll explain what causes this lump, how you can tell if it’s gone down, and when it’s time to call in an expert.
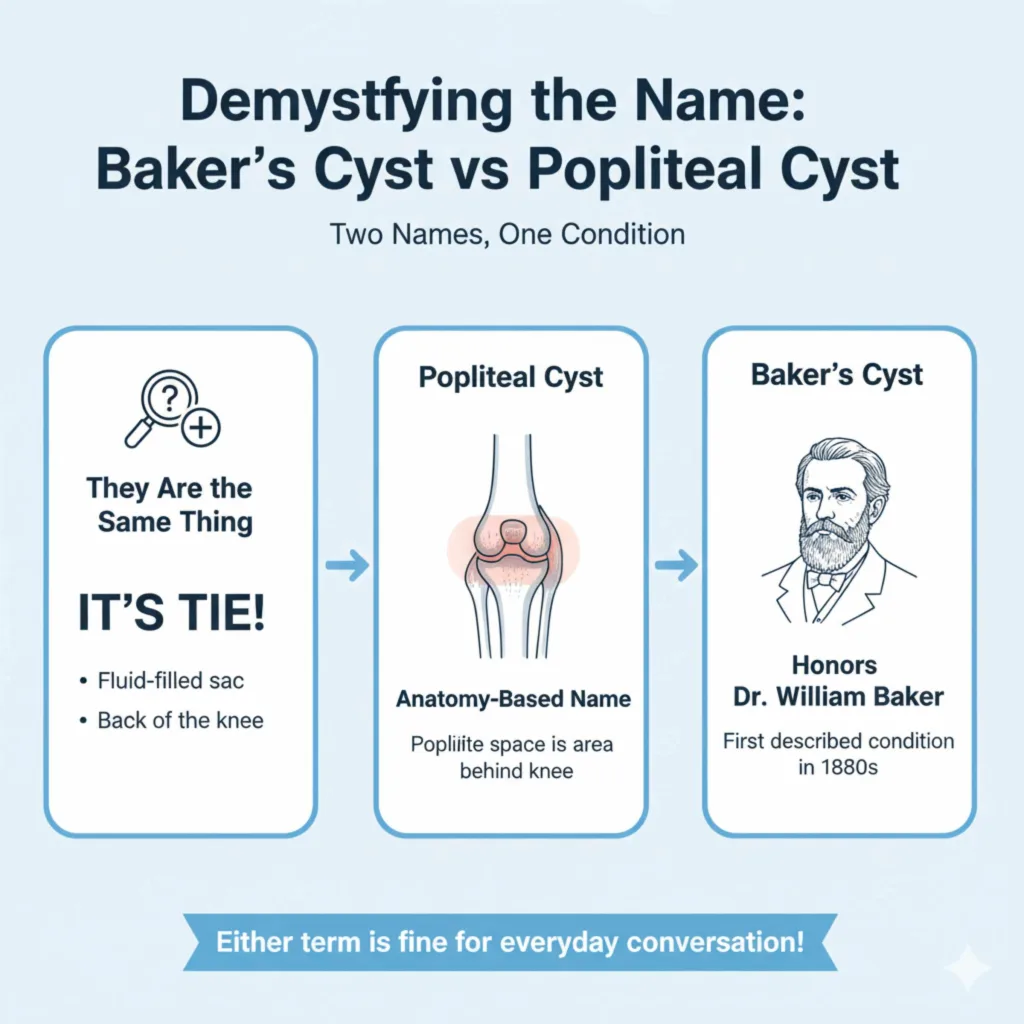
Demystifying the Name: Baker’s Cyst vs Popliteal Cyst
If you look up what causes this swelling, you’ll see two names floating around. This can make things frustrating when you are trying to research solutions. Let’s put those worries to rest right now.
They Are the Same Thing
This is the most important takeaway: Baker’s Cyst and Popliteal Cyst are just two different names for the exact same medical condition. They both describe a fluid-filled sac that pushes out from the back of the knee joint.
Why two names? It often comes down to where the name originated:
- Popliteal Cyst: This name is based on anatomy. The “popliteal space” is the proper medical term for the area directly behind your knee. So, a popliteal cyst is simply a cyst located in the popliteal area.
- Baker’s Cyst: This name honors Dr. William Baker, an English surgeon who first described this condition in detail in the 1800s.
For everyday conversation, you can use either term. Your doctor will know exactly what you mean! We will use both terms in this guide to make sure you recognize the language used everywhere you look for help.
What Exactly Is This Cyst? Understanding the Mechanics
To understand how to manage this issue, we need a quick, simple look at what’s happening inside your knee joint. Remember, this isn’t like a pimple; it’s related to the joint itself.
The Role of Synovial Fluid
Your knee joint is complex. To keep the bones moving smoothly—like good quality motor oil in an engine—the joint is lined with a thin membrane that produces a lubricating substance called synovial fluid. This fluid cushions your joints during activity.
When everything works right, the fluid stays inside the joint capsule.
How the Cyst Forms: A Simple Analogy
Imagine a balloon that is tightly connected to a pressurized hose. If the pressure in the hose gets too high, or if there is a weak spot in the balloon’s connection, a bulge forms.
A Baker’s (Popliteal) Cyst forms when:
- Too Much Fluid: The knee joint produces too much synovial fluid, often because the joint is irritated or damaged (this is the “high pressure”).
- A Leak or Bulge: This excess fluid squeezes out through a weak spot or a one-way valve in the back of the joint capsule.
- The Sac Forms: This trapped fluid creates a visible, compressible sac—the cyst—in the space behind the knee.
Crucially, the connective tissue between the cyst and the joint often acts like a one-way valve. Fluid can get out, but it struggles to get back in, causing the swelling to grow.
Why Do They Show Up? Common Causes of Knee Swelling
A popliteal cyst isn’t usually the main problem; it’s often a sign that something else is wrong inside the knee joint causing that extra fluid production. Think of it like an oil slick under your car—the slick itself isn’t the engine failure, but it shows the engine has a leak.
Primary Causes (The Root Issues)
The most frequent triggers that lead to the compression of fluid formation are related to joint wear and tear or previous injury:
- Osteoarthritis (OA): This is the most common cause, especially in older adults. As the cartilage wears down, the joint becomes inflamed and produces excess fluid.
- Rheumatoid Arthritis (RA): An autoimmune condition that actively attacks the joint lining, leading to significant inflammation and fluid buildup.
- Torn Meniscus: The menisci are C-shaped cartilage pads that act as shock absorbers. A tear can cause irritation and inflammation, triggering excessive fluid.
- Other Joint Damage: Ligament injuries (like an ACL tear) or cartilage damage can also irritate the joint lining enough to cause this backup.
Secondary Causes (Less Common in Adults)
In younger individuals, a popliteal cyst might form without a clear underlying arthritis issue. Sometimes, it just happens spontaneously due to minor damage or unusual anatomy, but this is less frequent.
Recognizing the Symptoms: What to Feel For
When you notice that bulge behind your knee, you might wonder, “Is this it?” Getting clear on the symptoms helps you decide the next steps.
Key Signs of a Baker’s Cyst
Since the cyst is located directly behind the knee, the symptoms are very localized:
- Visible Swelling or Lump: The most obvious sign. It feels soft, rubbery, and movable underneath the skin.
- Tightness or Fullness: Even if the lump isn’t huge, the area behind the knee can feel stiff, especially when straightening the leg completely.
- Pain Behind the Knee: Discomfort is common, especially during full knee flexion (bending) or extension (straightening).
- Pain in the Joint Itself: Because the cyst is connected to the knee, you might feel pain anywhere in the knee when you put weight on it.
- Cyst Size Changes: The lump might get larger if you are very active (producing more fluid) or slightly smaller if you rest.
Important Warning Sign: When the Cyst Breaks (Ruptures)
Sometimes, the pressure inside the cyst builds up so much that the tissue tears, causing the fluid to leak into the calf muscle space. This can be alarming!
If rupture occurs, you might suddenly feel:
- Sharp pain in the calf.
- Sudden swelling and redness in the calf area.
- Heat and tenderness in the calf, mimicking a blood clot.
Safety Note: If you suspect a rupture leading to severe calf swelling, redness, and pain, you must see a doctor immediately. While usually harmless, the symptoms strongly resemble a Deep Vein Thrombosis (DVT), a serious blood clot that requires urgent medical attention.
Comparing the Two Names: A Quick Reference Table
Since you came here looking for the distinction between “Baker’s Cyst vs Popliteal Cyst,” here is a simple table summarizing why the confusion exists but affirming their identical nature.
| Feature | Baker’s Cyst | Popliteal Cyst |
|---|---|---|
| Anatomical Location | Behind the knee (Popliteal Space) | Behind the knee (Popliteal Space) |
| Origin of Name | Named after Dr. William Baker (19th Century Surgeon) | Named after the anatomical region (Popliteal Fossa) |
| Underlying Cause Typical Link | Often linked directly to Arthritis or Meniscus Tear | Identical link to joint pathology |
| Treatment Approach | Focuses on treating the underlying knee problem | Identical—treat the source of the fluid |
Step-by-Step Home Care: Managing Minor Swelling
If the cyst is small, not overly painful, and your doctor has confirmed it’s not something serious like a DVT, you can absolutely manage the symptoms at home. These steps focus on reducing the irritation inside your knee, which is the only way to shrink the cyst naturally.
Phase 1: Reducing Inflammation (The First 48 Hours)
This phase is all about taking the pressure off the joint, much like letting a tire cool down before you try to fix the leak.
The R.I.C.E. Method for Your Knee
This classic approach works wonders for joint inflammation. For a beginner, remember RICE stands for Rest, Ice, Compression, and Elevation.
- Rest: This is the hardest part, I know! But you must limit activities that cause deep bending or impact, like running, squatting, or prolonged standing. If you work, try to sit more often or elevate your leg during breaks.
- Ice: Apply a cold pack wrapped in a thin towel to the area behind the knee or the front of the knee (where the pain might be originating) for 15 to 20 minutes, three to four times a day. Cold significantly reduces swelling and pain signals.
- Compression: Use an elastic bandage (like an ACE wrap) around the entire knee area. The compression helps prevent fluid from pooling in the back of the joint. Caution: Do not wrap so tightly that your foot becomes numb or blue.
- Elevation: When resting, prop your foot up higher than your heart level. Use several pillows. Gravity helps drain fluid away from the knee joint.
Phase 2: Gentle Movement and Knee Support
Once the initial sharp pain subsides, gentle movement is key. Stagnant joints get stiff, which leads to more pain.
- Gentle Knee Flexion/Extension: While sitting supported, slowly straighten your leg as far as comfortable, hold for a moment, and then slowly bend it. Repeat 10 times, three times a day. This helps pump the fluid gently back toward the main joint cavity.
- Over-the-Counter Relief: Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can help manage both the pain and the underlying inflammation in the joint. Always follow the package directions.
- Finding Proper Support: Sometimes, a quality neoprene knee sleeve can provide therapeutic warmth and gentle compression that feels supportive throughout the day while you are moving around.
When to Visit the Mechanic (I Mean, Doctor!)
While home care often handles minor swelling, some situations demand professional attention. If the problem is rooted in serious joint issues, simple home tricks won’t clear it up long-term.
Situations Requiring a Medical Consultation
You should schedule an appointment if you notice any of the following:
- The lump gets very large, very quickly (basketball size).
- The pain is constant and prevents normal walking or sleep.
- You have clear signs of infection: increasing redness, warmth, fever, or drainage from the skin over the cyst.
- You suspect the cyst has ruptured (severe calf pain/swelling). Please seek care quickly in this case.
- The swelling does not decrease at all after one to two weeks of dedicated home R.I.C.E. treatment.
Professional Treatments Explained Simply
If home care doesn’t work, your doctor might suggest one of these common solutions. The goal is always to fix the source of the fluid production.
| Treatment Method | What Happens | Why It Works |
|---|---|---|
| Aspiration and Injection | The doctor uses a needle to draw out the fluid and often injects a steroid (cortisone) into the joint. | Temporarily reduces joint inflammation, stopping the fluid production that feeds the cyst. |
| Treating the Primary Cause | If a meniscus tear is found via imaging (like an MRI), physical therapy or sometimes surgery addresses the tear. | Removing the source of the joint irritation stops the cycle of excess fluid creation. |
| Surgical Removal (Excision) | The surgeon makes an incision and physically removes the cyst sac entirely. | This is the most permanent fix, often reserved for very large, painful, or recurring cysts that do not respond to other treatment. |
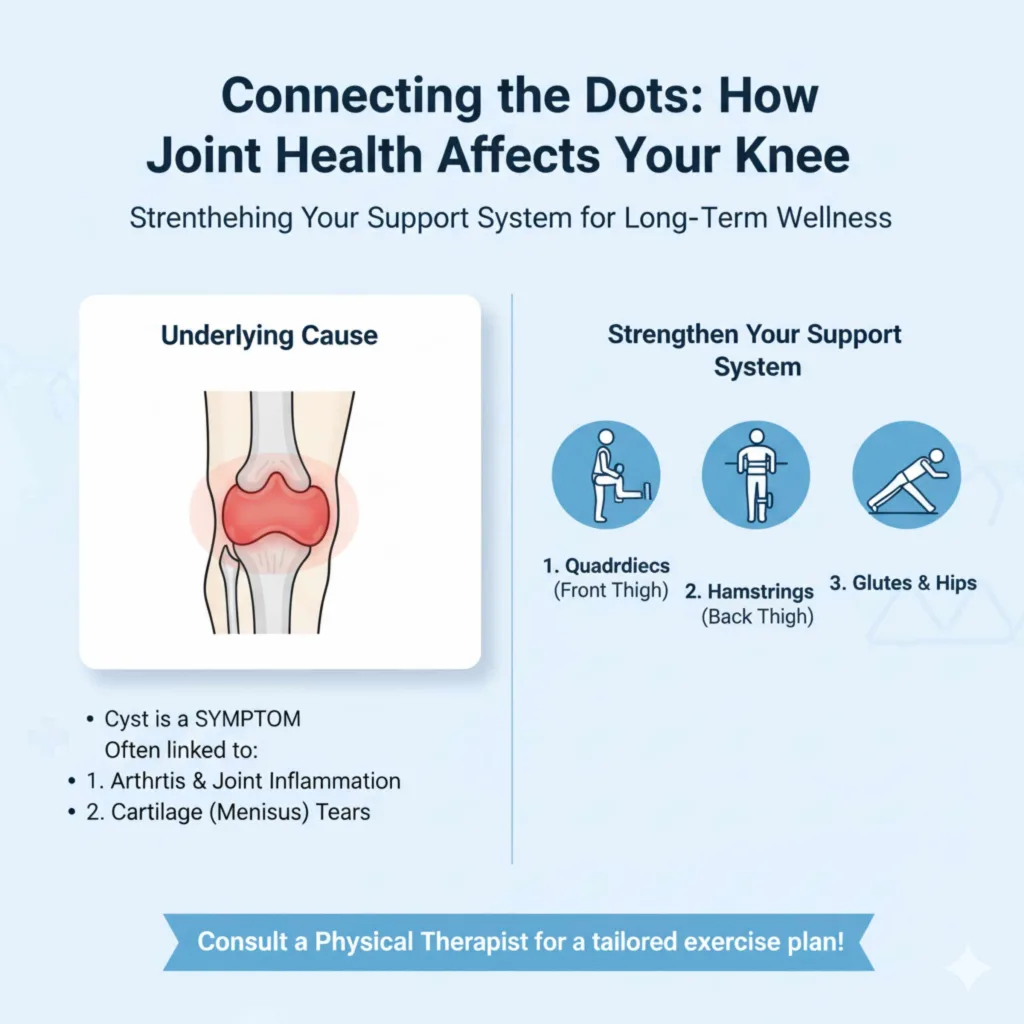
Connecting the Dots: How Joint Health Affects Your Knee
Since we established that the Popliteal Cyst is usually a symptom, focusing on overall knee health—especially joint cartilage—is your best defense against recurrence. Think about how you maintain your car’s suspension; healthy joints need care too. Organizations like the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) provide excellent ongoing advice on managing arthritis and joint pain, which is often the underlying driver.
Strengthening the Support System
Strong muscles act like external shock absorbers for your knee joint, reducing the stress that leads to inflammation. Focus on these areas:
- Quadriceps (Front Thigh): Strong quads absorb impact when you walk or climb stairs.
- Hamstrings (Back Thigh): These work with the quads to stabilize movement.
- Glutes and Hips: Weakness here causes the leg to track improperly, putting uneven stress on the knee joint.
It’s best to consult a physical therapist to get an exercise plan tailored to your specific knee strength level. Gentle strengthening exercises, like straight leg raises or heel slides, are great starting points.
Frequently Asked Questions (FAQ) for Beginners
Here are some common, straightforward questions that many people have when they first discover a lump behind their knee.
Q1: Can a Baker’s Cyst go away on its own without medicine?
Yes, often it can! If the underlying cause (like minor strain or temporary swelling) resolves, the fluid pressure drops, and the cyst may shrink or disappear completely, especially with a few days of rest and elevation.
Q2: Will getting a knee X-ray show the cyst?
Usually, no. X-rays show bones, not soft tissues like fluid sacs. Doctors typically rely on a physical exam, or sometimes an ultrasound or MRI, to definitively see the cyst and check for tears (like a meniscus tear).
Q3: Is it dangerous if a Baker’s Cyst ruptures?
While the cyst itself is not dangerous, a rupture causes fluid to leak into the calf, which can cause intense pain, swelling, and redness. Because these symptoms mimic a serious blood clot (DVT), you must get checked by a doctor right away to rule out the clot.
Q4: Can exercise make a Baker’s (Popliteal) Cyst worse?
Yes—the wrong kind of exercise can make it worse. High-impact activities like running, jumping, deep squats, or lunges increase pressure inside the knee joint and can cause the cyst to swell. However, low-impact movement (such as walking on flat ground, gentle stretching, and physical-therapy-guided strengthening) often helps by improving joint stability and reducing inflammation. The key is controlled, pain-free motion—not complete inactivity or aggressive workouts.
Q5: Does wearing a knee brace help a Baker’s Cyst heal?
A knee brace or compression sleeve won’t “cure” the cyst, but it can be very helpful for symptom relief. Light compression helps limit fluid buildup, improves comfort during movement, and provides a sense of stability. Braces are most effective when combined with rest, icing, and treatment of the underlying knee condition. Over-reliance on a brace without addressing joint health, however, won’t prevent recurrence.
Conclusion:
In the end, Baker’s Cyst and Popliteal Cyst are two names for the same condition—a fluid-filled swelling behind the knee caused by excess synovial fluid escaping the joint. The cyst itself is rarely the real problem; it’s a visible signal that something inside the knee, such as arthritis, a meniscus tear, or inflammation, needs attention.
Most cases are manageable with simple home care: rest, ice, compression, elevation, and gentle movement. When symptoms persist or worsen, medical treatment focuses on calming joint inflammation or correcting the underlying issue—not just draining the cyst. Understanding this connection empowers you to make smarter decisions, avoid unnecessary worry, and take action early.
Bottom line: Treat the knee, not just the lump. When joint health improves, the cyst usually follows!