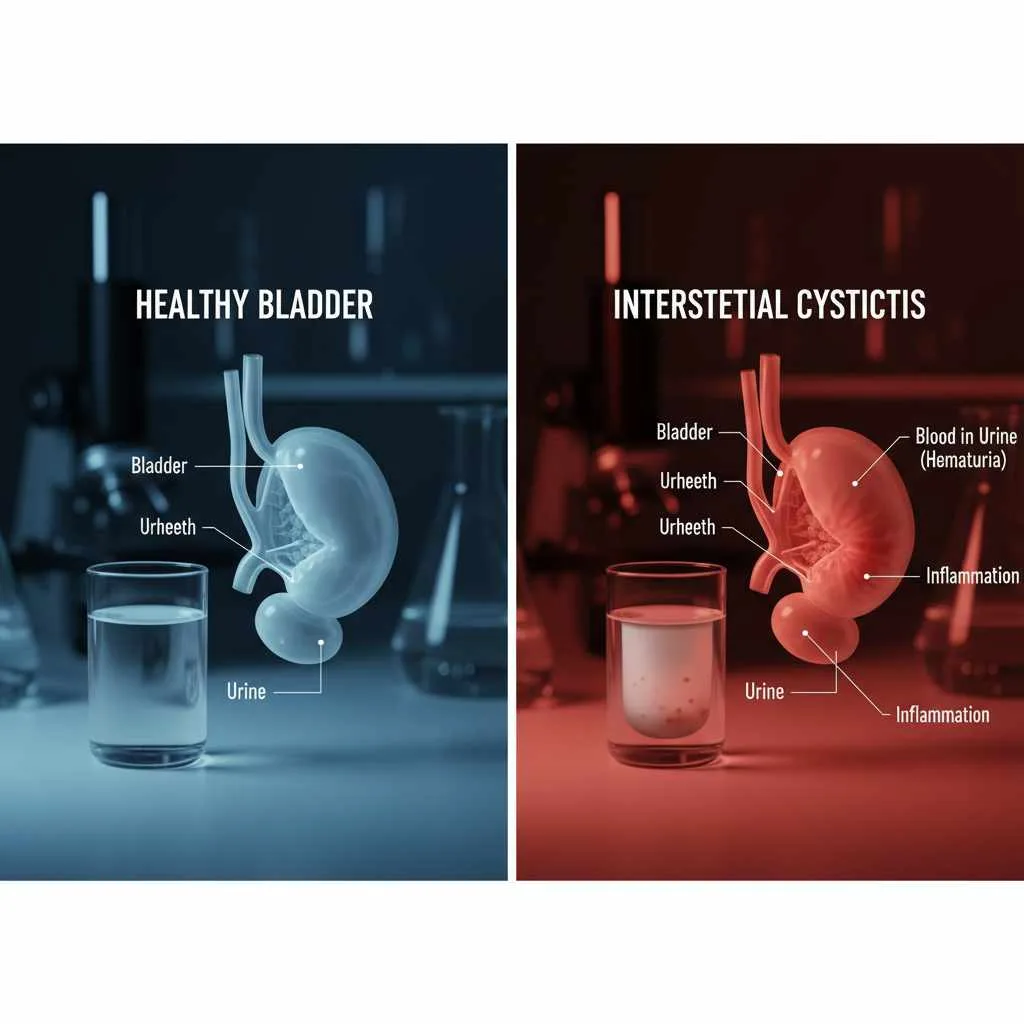
Yes, Interstitial Cystitis (IC) can sometimes cause blood in the urine, though it’s not a universal symptom and other conditions must be ruled out. Seeing blood in your urine, also known as hematuria, requires prompt medical attention to determine the cause and appropriate treatment for IC or other potential issues.
It’s completely understandable to feel worried if you notice blood in your urine. This can be a confusing symptom, especially when dealing with the ongoing challenges of Interstitial Cystitis (IC), also known as Bladder Pain Syndrome. You might be wondering if this is another symptom of IC or something else entirely. The good news is that understanding the connection between IC and blood in urine can help you feel more in control and know what steps to take next. We’re here to guide you through this, making it simple and clear, so you can focus on feeling better.
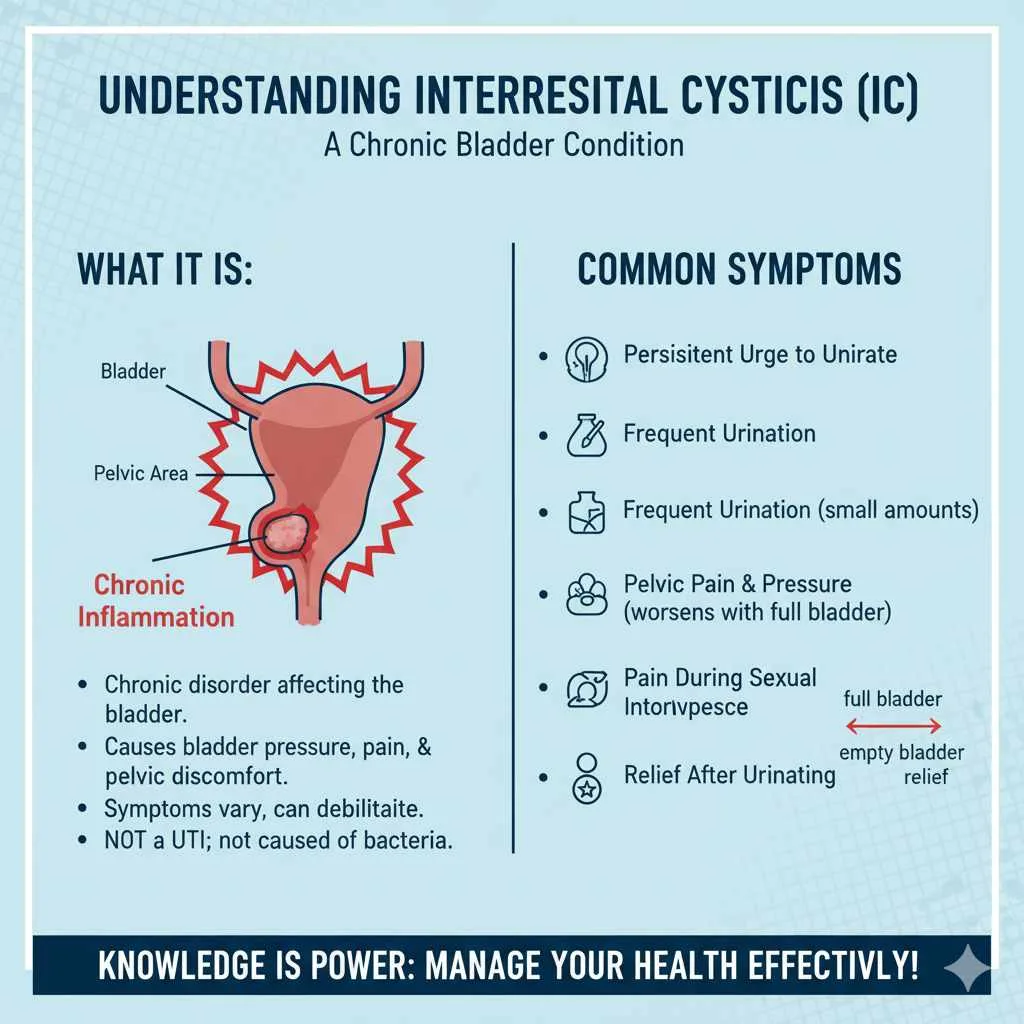
Understanding Interstitial Cystitis (IC)
Interstitial Cystitis (IC) is a chronic disorder that affects the bladder. It causes bladder pressure, bladder pain, and sometimes pelvic pain. The intensity of these symptoms can vary greatly from person to person and can change over time. For some, it’s a mild annoyance; for others, it can be debilitating. Unlike a typical urinary tract infection (UTI), IC is not caused by a specific germ and doesn’t always show up in standard urine tests.
What Are the Common Symptoms of IC?
The hallmark of IC is bladder pain that gets worse as your bladder fills and is often relieved, at least temporarily, by emptying the bladder. However, there’s a range of symptoms that people with IC might experience:
- Persistent urge to urinate
- Frequent urination, often in small amounts
- Pain and pressure in the pelvic area
- Pain during sexual intercourse
- Pain that worsens as the bladder fills
- Pain that improves after urinating
Does Interstitial Cystitis Cause Blood in Urine?
This is a very common and important question for individuals with IC. The short answer is: yes, Interstitial Cystitis can sometimes lead to blood in the urine (microscopic or visible hematuria). However, it’s crucial to understand that this is not a definitive or universal symptom of IC. Several factors within IC can contribute to blood in the urine:
- Inflammation: The chronic inflammation characteristic of IC can irritate the delicate lining of the bladder. This irritation can sometimes cause small blood vessels to break, leading to bleeding.
- Ulcers (Hunner’s Lesions): In about 5-10% of IC cases, a condition known as Hunner’s lesions (or Hunner’s ulcers) can be present. These are specific inflammatory patches or ulcers on the bladder wall. Hunner’s lesions are known to bleed relatively easily when touched or irritated during a procedure like a cystoscopy.
- Increased Bladder Sensitivity: The heightened sensitivity of the bladder in IC can make it more prone to trauma and subsequent bleeding from normal physiological processes that wouldn’t typically cause it in a healthy bladder.
Why Seeing Blood in Your Urine is a Red Flag
While IC can cause blood in urine, it’s essential not to assume that’s the sole cause. Hematuria, which is the medical term for blood in the urine, can be a sign of various other, sometimes serious, conditions. These can include:
- Urinary tract infections (UTIs)
- Kidney stones
- Kidney disease
- Bladder or kidney cancer
- Prostate problems (in men)
- Glomerulonephritis (inflammation of the kidney’s filtering units)
- Trauma to the urinary tract
Because of these possibilities, anytime you notice blood in your urine, whether it’s visible to the naked eye (gross hematuria) or only detected under a microscope (microscopic hematuria), it’s vital to consult a healthcare professional promptly. They can perform the necessary tests to determine the exact cause and rule out other conditions before attributing it solely to IC.
Diagnosing the Cause of Blood in Urine
When you see a doctor about blood in your urine, they will conduct a thorough evaluation. This process typically involves several steps to pinpoint the source of the bleeding.
Medical History and Physical Examination
Your doctor will start by asking detailed questions about your symptoms. This includes:
- When did you first notice blood in your urine?
- Is it visible or only detected by tests?
- Are there other symptoms like pain, fever, or changes in urination habits?
- Do you have a history of IC or other bladder/kidney conditions?
- Are you taking any medications?
A physical exam might also be performed to check for tenderness or other physical signs. For women, a pelvic exam may be necessary, and for men, a prostate exam might be included.
Diagnostic Tests
Several tests are commonly used to investigate hematuria:
- Urinalysis: This is usually the first test. It involves examining a urine sample to detect red blood cells, white blood cells, bacteria, and other substances. It can help identify infections or kidney inflammation.
- Urine Culture: If an infection is suspected, a urine culture can identify the specific bacteria causing it and determine which antibiotics will be most effective.
- Blood Tests: Blood tests can help assess kidney function and check for signs of infection or inflammation.
- Imaging Tests:
- Ultrasound: Uses sound waves to create images of the kidneys and bladder, looking for stones, masses, or structural abnormalities.
- CT Scan: Provides detailed cross-sectional images of the urinary tract, excellent for detecting kidney stones, tumors, or blockages.
- MRI: Can also provide detailed images and is sometimes used when CT scans are not suitable or for specific diagnostic questions.
- Cystoscopy: This procedure involves inserting a thin, flexible tube with a camera (cystoscope) into the bladder through the urethra. It allows the doctor to directly visualize the lining of the bladder and urethra. This is particularly important for diagnosing IC and identifying Hunner’s lesions. It can also help detect other bladder abnormalities like tumors or inflammation.
- Biopsy: If abnormal areas are seen during a cystoscopy, a small tissue sample (biopsy) may be taken for examination under a microscope.
IC Management and Its Impact on Hematuria
If blood in your urine is confirmed to be related to Interstitial Cystitis, managing your IC is key to reducing or eliminating this symptom. The treatment approach for IC is often multi-faceted and aims to reduce inflammation, manage pain, and improve bladder function.
Treatment Options for Interstitial Cystitis
These treatments can help calm the bladder lining and potentially reduce bleeding.
- Lifestyle and Dietary Changes: Many people with IC find that certain foods and drinks can trigger or worsen their symptoms. Common triggers include acidic foods, caffeine, alcohol, spicy foods, and artificial sweeteners. Keeping a food journal can help identify personal triggers. Stress management techniques are also beneficial.
- Oral Medications:
- Pentosan Polysulfate Sodium (Elmiron): This is the only oral medication specifically approved by the FDA for the relief of IC pain. It’s thought to help by restoring the GAG layer of the bladder.
- Antihistamines: Medications like hydroxyzine can help reduce bladder inflammation and urgency.
- Tricyclic Antidepressants: Drugs like amitriptyline can help relax the bladder and block pain signals.
- Pain Relievers: Over-the-counter pain relievers or prescription medications may be used for pain management.
- Bladder Instillations: A solution is placed directly into the bladder via a catheter. Common solutions include dimethyl sulfoxide (DMSO), heparin, lidocaine, or a combination of medications. This delivers medication directly to the inflamed bladder lining.
- Physical Therapy: Pelvic floor physical therapy can be very helpful for relieving pelvic pain and muscle tension associated with IC.
- Nerve Stimulation: Techniques like sacral nerve stimulation (SNS) and transcutaneous electrical nerve stimulation (TENS) can modulate nerve signals to the bladder, helping to reduce pain and urinary frequency.
- Surgery: Surgery is typically a last resort for IC patients, reserved for severe cases where other treatments have failed. It might involve removing scar tissue, cauterizing Hunner’s lesions, or in rare cases, removing the bladder.
Dealing with Hunner’s Lesions
If Hunner’s lesions are identified during a cystoscopy, they can often be treated directly. Treatments aim to remove or reduce the inflammation of these lesions:
- Cauterization: The lesions can be burned away using electrical heat or lasers.
- Fulmination: Similar to cauterization, this uses electrical current to destroy the tissue.
- Surgical Excision: In some cases, the lesions can be surgically cut out.
These procedures can significantly reduce pain and bleeding associated with Hunner’s lesions and may lead to symptom improvement for a period, sometimes requiring repeat treatments.
Important Considerations When Experiencing Hematuria with IC
It’s crucial to approach any instance of blood in your urine with a proactive mindset. Here are some key things to keep in mind:
- Don’t Ignore It: Even if you have IC and have experienced similar symptoms before, recurring or new instances of blood in urine should always be evaluated by a healthcare provider.
- Communicate with Your Doctor: Be very specific when describing your symptoms. Mention the color of your urine, any associated pain, frequency of urination, and any new or worsening IC symptoms. Also, inform them about all medications and supplements you are taking.
- Stay Hydrated (with water): Unless advised otherwise by your doctor, drinking plenty of water can help dilute your urine and flush out your urinary system, which can be beneficial. However, if you have IC, you’ll need to balance hydration with avoiding irritants – water is usually safe.
- Follow Your Treatment Plan: Adhering to your prescribed IC treatment plan is crucial for managing overall bladder health and can indirectly help prevent or reduce episodes of hematuria.
- Be Patient: The underlying causes of IC and hematuria can be complex. Diagnosis and finding the most effective treatment might take time and persistence.
When to Seek Immediate Medical Attention
While not all blood in urine is an emergency, certain signs warrant immediate medical care. Seek emergency help if you experience any of the following:
- Severe pain during urination
- Inability to urinate
- Fever and chills along with blood in urine
- Sudden and severe flank or abdominal pain
- Dizziness or weakness
Living with IC and Hematuria: Hope and Support
Living with a chronic condition like Interstitial Cystitis can feel overwhelming, especially when new or concerning symptoms like blood in the urine appear. However, it’s important to remember that you are not alone, and effective management is possible. Significant advancements have been made in understanding and treating IC, offering hope for improved quality of life.
By working closely with your healthcare team, actively participating in your treatment, and seeking support from others who understand, you can navigate the challenges of IC and hematuria. Organizations like the Interstitial Cystitis Network and the American Urological Association Patient Resources offer valuable information and support communities.
Frequently Asked Questions (FAQ) about IC and Blood in Urine
Q1: Is blood in my urine always a sign of a serious problem with IC?
No, not always. While IC can cause blood in urine due to inflammation or Hunner’s lesions, it is crucial to let your doctor evaluate it. Other common causes like infections or stones need to be ruled out, and sometimes, IC itself is the cause. Prompt medical assessment is always recommended.
Q2: How can I tell if the blood in my urine is from IC or something else?
You can’t tell just by looking. A healthcare professional uses medical history, physical exams, and diagnostic tests (like urinalysis, imaging, and cystoscopy) to determine the cause of blood in your urine. IC symptoms often include bladder pain, urgency, and frequency, which can help doctors in diagnosis.
Q3: If my IC is well-managed, will I stop seeing blood in my urine?
Effective management of IC can often reduce or eliminate symptoms, including inflammation that might lead to blood in the urine. However, if Hunner’s lesions are present, direct treatment of those lesions might be needed even with general IC management.
Q4: Should I stop my IC medications if I see blood in my urine?
No, never stop or change your medications without consulting your doctor. Your IC medications are likely prescribed to manage your condition. If you see blood in your urine, contact your doctor to discuss it; they will advise you on the best course of action regarding your medications.
Q5: How long does it take for blood in the urine to go away if it’s related to IC?
If the blood is due to inflammation or minor irritation of the bladder lining from IC, it might resolve as the inflammation subsides with treatment. If it’s related to Hunner’s lesions, it will likely only resolve after the lesions are treated directly through procedures like cauterization or excision, as performed during a cystoscopy.
Q6: Can certain treatments for IC cause blood in the urine?
Generally, the treatments themselves are designed to help the bladder, not harm it. However, the diagnostic procedures, like a cystoscopy, where the bladder lining is examined directly, may cause temporary, minor spotting of blood. It’s very unlikely that standard oral medications or bladder instillations would directly cause blood in the urine unless there’s a complication.
Conclusion
Experiencing blood in your urine while living with Interstitial Cystitis can be a significant source of worry. It’s important to know that while Interstitial Cystitis can indeed cause hematuria due to inflammation or the presence of Hunner’s lesions, it is crucial not to assume this is the only cause. The presence of blood in the urine is a signal that demands a thorough medical evaluation to rule out other potential conditions. By collaborating closely with your healthcare provider, undergoing necessary diagnostic tests, and adhering to a tailored treatment plan for your IC, you can gain clarity and effectively manage your health. Remember, maintaining open communication with your doctor and seeking support are vital steps toward achieving better bladder health and an improved overall quality of life.